A parachute pack for families of a child newly diagnosed with TSC
It is estimated that 1 child in every 6,000 has TSC (Tuberous Sclerosis Complex). This free booklet will help you understand TSC, what causes it, how it might affect your child, TSC tests and treatments and support that is available to you and your family.
The information is available below, and as a downloadable, print-at-home pdf (please fill out the form).
We sincerely hope that this parachute pack will help you through this difficult time.
Parachute pack for families of a child newly diagnosed with TSC
You have been given this booklet because your child has been diagnosed with TSC (Tuberous Sclerosis Complex). Like most people, you may have never heard of TSC before. TSC is a genetic condition that causes different signs and symptoms in each person who is affected.
Having a child diagnosed with TSC is a shock. Many parents are overwhelmed by their feelings, including being confused by information about TSC, being afraid of what the future will hold and being sad about the dreams they had for their child that may now seem out of reach. You may be feeling something similar.
Some parents describe this experience as being in ‘free fall’. This is the reason we have called this resource a parachute pack. We hope it will help you through this difficult time. There is no correct way to feel or act when you find out your child has TSC. Some people want to learn everything they can about TSC and will spend hours reading about new research or stories of people living with TSC. Other people find they are not ready to learn more about TSC for many weeks, months or even years.
It is possible for TSC to cause growths to develop in many organs of the body, including the brain, skin, heart, lungs and kidneys. TSC can also cause epilepsy, developmental delay and autism. However, TSC affects each person differently. Even people who share the same TSC gene change can have different signs and symptoms of TSC. There is no reliable way to predict how TSC will affect your child.
In the last 10 years research has changed the way we understand, manage and treat this complicated disease. This means your child can benefit from new treatments which can reduce the impact TSC will have on their life.
Progress started in the 1990s when the genes that cause TSC were discovered. This led to the first medicines specifically for TSC being approved in Australia in 2013. Research has also refined the use of other treatment options for TSC. The medical approach to TSC is changing – from a focus on treating symptoms as they arise to a focus on active monitoring and trying to prevent signs and symptoms from occurring.
This parachute pack will help you to understand TSC and what you can do to help your child have the best life possible.
If your child has not yet been born, we recommend our parachute pack for families of an unborn baby with possible TSC (Tuberous Sclerosis Complex).

I can remember hearing the words ‘Tuberous Sclerosis’ for the first time when Michelle was pregnant with Oliver. We were confused and afraid of what our child’s future would be. If I could go back in time, I would tell myself that, despite the challenges of the future, you will still enjoy the journey. You have a lot to learn but your child is really not any different to any other child. They will have their own personality and they will have so much joy in their life.
It is easy to be overwhelmed by what you read about TSC. This is the reason many doctors will still tell parents: ‘Do not google TSC’. There are many reasons why the information you read may cause you distress.

- Many of the stories you read online about people living with TSC will be from people where TSC has had a significant impact on their life. When TSC has caused severe symptoms such as difficult to control epilepsy and disability, people are more likely to share their stories and get involved in organisations like TSA (Tuberous Sclerosis Australia). It may help you to remember that many people with TSC are mildly affected and simply living their lives and not discussing their TSC in public forums.
- Even factual information can give the impression that TSC always causes a lot of different medical conditions. Remember, most people with TSC will not experience all signs and symptoms.
- Some information is out of date. The outlook for a child born with TSC today is different to a child born a generation or even ten years ago. This is because we have a better understanding of TSC. Now we are able to look for signs and symptoms of TSC before they cause problems and minimise their impact with several different treatment options.
When my son Koby was born, the information I found online via search was confronting and scary, and it seemed to focus only on the worst case scenario. The TSA website is a much better starting point for people needing information.
You may find it helpful to read some of the stories below from our TSC Community.
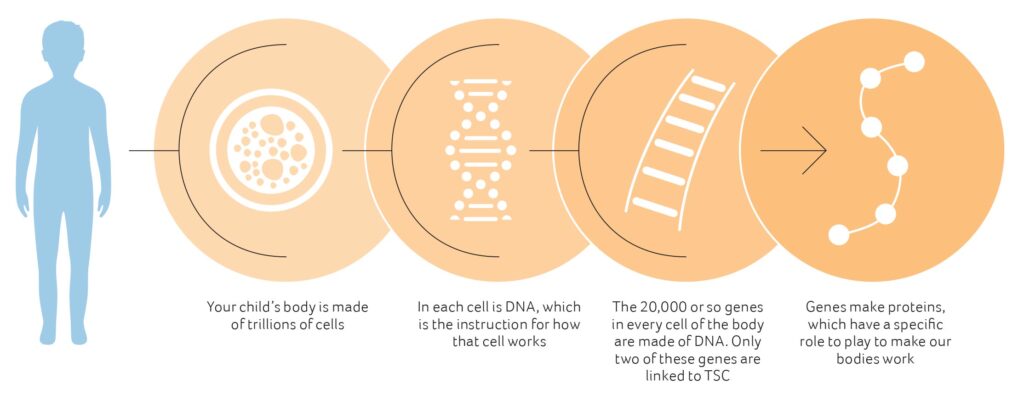
First, a gene change
Your child has TSC because they have a change in either their TSC1 or TSC2 genes. These changes are sometimes called ‘mutations’. All of our bodies contain many gene changes, but only some of them are known to cause genetic diseases.
There are two possibilities for how your child’s gene change occurred:
1. The gene change was passed onto your child, from either their mother or father who also has TSC
OR
2. The gene change occurred around the time your child was created from an egg and a sperm. This is often called a ‘spontaneous mutation’. In this case, your child is the first person in the family to have TSC.
Around two-thirds of children born with TSC have a spontaneous mutation. It may not be clear whether this is the case in your family. A genetics service can help you understand how your child’s gene change occurred.
Second, the gene change causes cells to grow differently
The TSC gene change stops the gene from producing the protein that the body needs to control cell growth. This is why TSC often causes clusters of cells to grow more than they should. The growths that TSC causes are the result of too many cells growing or cells growing more than usual.
TSC1 and TSC2 work together to control cell growth. This is why a gene change in either of these two genes can cause a person to have TSC.
Why is TSC called TSC?
The name Tuberous Sclerosis comes from how one cluster of abnormal brain cells of TSC was first described by doctors. They described these abnormal cells as looking similar to a potato – a ‘tuber’. The medical word for ‘hard’ is ‘sclerosis’, derived from a Greek word. This is how the name ‘Tuberous Sclerosis’ came into being.
Medical research revealed that people with TSC had many different signs and symptoms, not just tubers in their brain. The term ‘Tuberous Sclerosis Complex’ was adopted to reflect the fact that a number of different organs may be involved in TSC. The acronym TSC is also helpful to distinguish from other ‘TS’ conditions such as Tourette’s syndrome and Turner’s syndrome. It is common for doctors and people living with TSC to refer to the disease as simply Tuberous Sclerosis.

We had to face everything else that comes with a diagnosis of TSC. The doctors appointments, scans, blood tests and all of the emotional upheaval. It was very overwhelming. Although our story sounds challenging and at times very sad, Alana is one of the strongest and happiest children you will ever meet
Genes Make Proteins
How is TSC diagnosed?
There are two different ways that TSC can be diagnosed:
1. When a person has signs and symptoms of TSC in their body (clinical diagnosis)
2. When a person has a TSC1 or TSC2 gene change that is known to cause TSC (genetic diagnosis).
1. Clinical diagnosis: Diagnosing TSC by signs and symptoms
This is the way most people are diagnosed with TSC. Doctors look for signs of TSC in different parts of the body, including the skin, brain and kidneys. Some signs can be seen with just a physical exam and others require images to be taken by ultrasound or MRI.
If someone has some signs of TSC, but not enough for a diagnosis, they may be considered to have ‘possible TSC’.
Doctors may arrange a genetic test to look for a TSC1 or TSC2 gene change. They may also suggest that more tests are done in the future to look for signs of TSC that may become visible later, such as those in the heart or eyes.
2. Genetic diagnosis: Diagnosing TSC by TSC1 or TSC2 gene change
TSC can be diagnosed if a specific change in either the TSC1 or TSC2 gene is found. Genetic testing is usually done through a blood test and DNA is analysed in a laboratory, either here in Australia or overseas.
If a person is given a clinical diagnosis of TSC, a genetic test is not needed. In fact, many people with TSC have never had a genetic test. Genetic testing can be useful to understand if the person with TSC is the first person in their family to have TSC or if they have inherited a TSC gene change from their father or mother.
A clinical genetics service can help you with questions such as ‘How did my child get TSC?’ and ‘Will it affect other people in my family?’ They can discuss the usefulness of genetic testing for your family and the different tests that are available.
Because there are so many areas of the body that could be affected by TSC, I found not knowing how our little girl would be hard to deal with.
This section highlights the signs and symptoms of TSC that are most common in early childhood. It will take you some time to become familiar with medical terminology related to TSC. You may find it helpful to concentrate on just the terms on this page to avoid becoming overwhelmed.
TSC may cause changes in your child’s brain
It is possible that your child with TSC will have one or more different types of changes in their brain. Some of these cause problems and some do not.
1. Cortical tubers grow in the part of the brain surface called the cerebral cortex. Around 80% of people with TSC have cortical tubers. These form in the womb, grow along with the brain and do not get bigger over time. Cortical tubers may be the source of epilepsy.
2. Subependymal nodules (SENs) are small growths found on the surface of the part of the brain called the cerebral ventricles. Around 80% of people with TSC will have at least one SEN. SENs can grow and once they grow larger than one centimetre, they are classified as a SEGA.
3. Subependymal giant cell astrocytomas (SEGAs) are large SENs. They are clusters of abnormal cells that occur in one in ten people with TSC. SEGAs usually grow slowly, but if they keep growing they can cause serious problems. SEGAs can be seen on an MRI, so this test is done regularly to monitor for SEGA development or growth.
4. Other changes can affect how brain cells connect with each other. This can affect learning and can lead to autism in some children with TSC.

TSC may cause seizures
Your child with TSC is at risk of having seizures and being diagnosed with epilepsy, particularly in the first two years of their life. A seizure can occur when a cortical tuber produces an abnormal electrical discharge in the brain. This discharge can spread to other parts of the brain and cause their normal functions to be abnormally activated, such as brain cells that cause arms and legs to move.
There are many different types of seizures. Some of the seizures that young children with TSC experience can go undetected.
Frequent seizures in babies and very young children can interfere with normal brain development or learning. Seizures can also lead to accidents when a child cannot control their body. This is why it is very important to prevent or control seizures. One way this is done is by regular EEG tests to look for early signs of seizures in babies and very young children with TSC.
TSC may cause challenges with learning
Many, but not all, children with TSC will require additional support to learn. Your child with TSC is more likely than children without TSC to have delays to their development, specific learning difficulties and autism. However, many children with TSC also have normal learning ability. Monitoring your child’s development and intervening early with therapy and seizure control, can all reduce the chance of your child having learning challenges.
TSC may cause changes in your child’s heart
Your child with TSC may have changes to the cells in their heart. These clusters of abnormal cells are called cardiac rhabdomyomas. These may have grown while your child was growing in the womb but will have stopped growing after your child was born. In most cases, they start to shrink after birth.
In some babies, these growths affect how blood flows through the heart or cause heart rhythm problems. Medication to help the heart or shrink the rhabdomyomas quickly, can assist. It is rare that surgery is required.
TSC can cause changes to other parts of your child’s body
TSC may also cause changes to cells in other parts of your child’s body. These include the eyes, skin, kidney and lungs. Many of these will not cause problems. For those that do, there are treatments available.
These changes may happen as your child gets older. This is why there is a list of recommended tests that will be repeated regularly to look for these changes and help decide if any treatment is required.

We feel confident the early diagnosis and intervention Oskar received has helped him have the very best start to life with TSC
Because TSC can affect many different parts of the body and many different aspects of a person’s life, a number of health professionals are involved in the person’s care. The team will change depending on:
- The age of the person with TSC
- Which signs and symptoms of TSC affect the person
- How health care is organised in your local area.
While your child is young, their core care team may include:
- Paediatrician – a doctor with special training in the health of children
- Neurologist – a doctor with special training in the brain and nervous system
- Geneticist and/or genetic counsellor – health professionals with special training in genes and genetic diseases. They can help you to understand if any other members of the family are affected by TSC and support your family when you are planning more children.
- Early intervention therapists – these can include early intervention teachers, physiotherapists, occupational therapists and speech pathologists.
The importance of expert centres
TSC is a relatively rare condition, so not all health professionals have accurate and up to date knowledge about it. TSA maintains a list of health professionals in Australia called the TSC Health Care Professionals Network who we know have up to date knowledge about the disease. These health care professionals like to see children with TSC as soon as possible so that they can plan tests and ongoing monitoring.
If you are unsure about whether your doctor has up to date knowledge of TSC, you can:
- Provide them with information from TSA
- Talk to TSA’s Nurse about your child’s health care to check against the latest research and clinical guidelines
- Ask your doctor to review your child’s case with a member of the TSC Health Care Professionals Network
- Ask for a second opinion from a different doctor, perhaps someone who is a member of the TSC Health Care Professionals Network.
Living outside a capital city
Many children with TSC visit specialists in a capital city. Each state and territory has a scheme that provides financial assistance for families living in regional areas who need to travel for their health care.
Australian Capital Territory – Interstate Patient Travel Assistance Scheme
New South Wales – Isolated Patients Travel and Accommodation Assistance Scheme
Northern Territory – Patient Assistance Travel Scheme
Queensland – The Patient Travel Subsidy Scheme (PTSS)
South Australia – Patient Assistance Transport Scheme
Tasmania – Patient Travel Assistance Scheme (PTAS)
Victoria – Victorian Patient Transport Assistance Scheme (VPTAS)
Western Australia – Patient Assisted Travel Scheme (PATS)
The National Disability Insurance Scheme (NDIS)
Depending on how TSC affects your child, you may be eligible for the NDIS. An NDIS funding package can help you access early intervention and other disability supports.
Early childhood early intervention (ECEI)
Early intervention means doing things as soon as possible to support the development and wellbeing of children with a disability. This can be important for children with TSC because they are more likely to have delays in their development than a child without TSC.
More information:
https://raisingchildren.net.au/disability/ndis/ndis-early-intervention/early-intervention-ndis
https://www.ndis.gov.au/understanding/families-and-carers/how-ecei-works-step-step-process
Ongoing supports
Some people with TSC have one or more disabilities. The NDIS can provide supports for people with TSC to achieve their goals.
TSC is included in a list of conditions recognised by the NDIS as a permanent condition where further assessment is needed to determine how much it affects the person. This means your child will require reports from one or more health professionals before they can access the NDIS.
If your child is found eligible, they will be given a package of funding that can be used to purchase the support they need.
More information:
https://www.ndis.gov.au/participants
https://www.thegrowingspace.com.au/library/
https://www.amaze.org.au/wp-content/uploads/2019/10/AMZ_NDIS_booklet
Coordinating care
With lots of different health professionals involved in caring for a person with TSC, some coordination is required. Most frequently, it is the parents of a child with TSC who do most of the coordination of health care appointments. Other coordination may be provided by:
- Your paediatrician, who will play a critical role in communication between health care professionals and managing referrals
- One key specialist, usually a neurologist, who may coordinate tests and appointments to monitor all the signs and symptoms of TSC, not just in the brain
- A nurse provided by the hospital who may be able to provide care coordination. They could be known as ‘nurse navigators’ or ‘connected care services’.
Keeping records
All of these different appointments, tests and doctors can create lots of information to keep track of. You may need to come up with a system of keeping records that works for you and your family.

We have a little book for Caleb, where we write down all his appointments, everything that happens to Caleb in hospital, all the information we have learnt from talking to TSA. I feel really nerdy about it, but it is a great support for us to have this. Our brains are just so full of everything, it is hard to remember. When a nurse commented: ‘Miriam is really organised, she won’t forget this stuff’, this was the first time I felt that I wasn’t a pain, that I am actually doing something
When your child is first diagnosed, they will have a series of tests – based on international guidelines – to help understand how TSC is currently affecting them. These are known as ‘baseline tests’. The results of these important tests will help your child’s doctors identify any treatments that are required. They will also be used in the future to compare results to see what has changed.

Obtain a baseline routine electroencephalogram (EEG); if EEG is abnormal, and particularly if features of TAND are present, follow this with 24-hour video EEG to look for subtle seizure activity.

Undergo magentic resonance imaging (MRI) of the brain to look for possible tubers, subependymal nodules (SENs) and subependymal giant cell astrocytomas (SEGAs).

Obtain a routine electrocardiogram (ECG) to check for abnormal heart rhythm. Obtain an echocardiogram to assess cardiac function and presence of rhabdomyomas (especially in children under 3 years of age).

Have an assessment for TSC-associated neuropsychiatric disorders (TAND), a new terminology to describe the interrelated behavioral, intellectual, and neuropsychiatric features commonin TSC. Download the TAND Checklist designed to be completed by a clinician.
Review the newly diagnosed individual’s nearest three generations (siblings, parents, and either children or grandparents). Genetic testing or family counselling when TSC diagnosis is in question should be offered.

Undergo an exam by an ophthalmologist for possible vision problems or abnormalities of the retina.
The international guidelines make reference to performing MRI of the abdomen to check for possible renal angiomyolipomas or cysts. In Australia, an ultrasound/imaging of the kidneys is much more commonly used in place of an MRI of the abdomen. Kidney function (glomerular filtration rate, or GFR) and blood pressure should be measured.

Undergo dermatological and dental examinations to check for abnormalities of the skin and teeth that are frequently associated with TSC.

Additional Recommendations for Newly Diagnosed Infants and Children (Under 3 Years of Age)
Teach parents and other caregivers of children under 3 years of age about how to recognize focal seizures and infantile spasms and what to do if they suspect the child is having seizures. More information and links to videos are available at TSC Alliance
Ongoing surveillance
Many of these tests are repeated at regular intervals. There are also other tests done as your child gets older. These tests aim to find signs and symptoms of TSC as early as possible to allow for early treatment when required.
Visit our information page for the full list of tests for baseline and ongoing surveillance:
Early tests for seizures
If your child has not yet had a seizure, it is recommended to look for early signs of seizures using an EEG test. An EEG measures the electrical activity within the brain using small metal discs stuck onto the outside of a child’s head.

An EEG may show abnormal electrical charges in the brain before your child has their first seizure. It may be possible to treat these electrical charges and so reduce the chance of your child developing troublesome seizures.
Vigabatrin (also called Sabril)
Vigabatrin is a medication that is very effective for controlling seizures in young children with TSC, including infantile spasms. Because stopping a young child’s seizures and the effects seizures have on the developing brain is important, this medication is recommended as the first choice for treating seizures in TSC, including infantile spasms. Your doctors will help you weigh up the risks of this medication with its benefits.
Epilepsy surgery
In some children with TSC there is a single tuber starting most seizures. Surgery to remove this tuber may be the best way to control seizures. Your child’s neurologist will be able to talk to you about whether surgery is an option for your child.
mTOR inhibitors (also called Afinitor, Everolimus, Sirolimus and Rapamycin)
These are relatively new medicines for TSC that can shrink some clusters of abnormal cells and treat some types of epilepsy caused by TSC. Ongoing research projects are helping to understand when a person with TSC can benefit most from these medicines.
An mTOR inhibitor skin cream can be used to treat bumps, called angiofibromas, which can grow on the face of a child with TSC. This skin cream can be used as soon as these small bumps appear and prevent the angiofibromas from forming.
You can discuss these treatments and others with your health care team or contact TSA for more information.

I believe the early intervention helped Koby enormously with seizure control. It has helped him be the best version of himself that he can be.
TSC is complicated. As a parent of a child with TSC you will learn a lot about TSC and become an expert on your child.
Australia’s health, education and disability services can be wonderful, but sometimes they work best when a parent advocates strongly for what their child needs. Parents of children with TSC learn to ask for what their child needs and keep asking to ensure their child gets access to the services and care they need.
Your journey to being a parent expert and advocate has just begun.
Emotional support
You and your family will need time and support to adjust to life with TSC. You may have hopes and dreams for your child that may feel out of reach now. You may be feeling alone and scared about what the future will hold. Emotional support may come from your friends, your family and from professionals.
Most families with TSC seek some professional support for their mental health at some point.
You can seek support from a psychologist, a counsellor or a support group. Your GP can help you connect to a local psychologist through a mental health plan.
Telling friends and family
It can be a daunting task to share your child’s TSC diagnosis with your friends and family. You may choose to wait until you have more information about how TSC will affect your child or what their health care plan is going to be before you do this.
You may find that some friends and family cope better with this news than others. You may find that through this experience you connect with new people and find support in unexpected places.
A sample email announcement
Dear friends and family,
We are writing to let you know that our baby girl, Olivia, has been diagnosed with a genetic condition called Tuberous Sclerosis Complex (TSC). This means that she has a genetic change causing some of her cells to grow differently. TSC may cause her some health complications during her life. It is difficult to predict how TSC will affect her but we know she will require lifelong monitoring to keep her healthy.
We are still learning about TSC ourselves so we probably won’t be able to answer all of your questions at the moment. You can learn more about TSC through the website of TSA (Tuberous Sclerosis Australia) at www.tsa.org.au
We are happy and proud parents and we would like you to see her as we do. She is, quite simply, our beautiful baby girl. We wanted to give you time to adjust to the news, so you won’t feel the need to have an immediate response. Adjusting to life with TSC is not easy and we know we will need our friends and family to support all of us.
We’d like you to treat Olivia just like any other child. We would like to encourage you to call us, and come to see her. She sleeps, eats, cries and needs her nappy changed, just like every other baby! Please feel free to come and give her a cuddle.
TSA is here to help you and your child
TSA (Tuberous Sclerosis Australia) can provide you with information and support in various forms.
Telephone Nurse Service
This is a free, confidential information and support service which provides TSC information and links to practical support.
You may like to book an appointment with our Nurse to discuss:
- finding the right health professionals to provide care for you and your baby
- the tests and treatments that you and your baby may need to have
- how you are feeling about your child’s possible diagnosis
You can book a time to talk with TSA’s Nurse by completing the booking form, by emailing [email protected] or by calling 1300 733 435 (Australia only).

Right from that first phone call, TSA has been essential to our life with TSC. At no time has TSA told me what to do, but I have been able to come back and ask them what they think about the options we have. They have helped our family make life changing decisions and be confident in these decisions.
Detailed information pages
TSA publishes medically reviewed information pages and a rich set of resources and articles about TSC. These are regularly reviewed and updated to ensure the information is both current and accurate. When you are ready you can access these here.
Education events
TSC conferences, seminars and workshops are held around Australia. These provide opportunities to hear from experts in TSC and connect with other people in Australia living with TSC. Travel subsidies are often available.
Connecting on Facebook
TSA runs a closed discussion group on Facebook.
At any time, you can contact TSA by calling 1300 733 435 (Australia only) or emailing [email protected]. We encourage you to contact our team to learn more about TSC, the work of TSA and to connect with other organisations, other families and/or health professionals that can help you and your child.
Last updated: 30 January 2023
Prepared by: Clare Stuart and Jackie Gambrell, TSA (Tuberous Sclerosis Australia); Dr Clara Chung, Clinical Geneticist, Sydney Children’s Hospital
Reviewed by: Dr Kate Riney, Paediatric Neurologist and Epileptologist and Lead Clinician Queensland TSC Clinic, Queensland Children’s Hospital, Brisbane; Dr John Lawson, Paediatric Neurologist and TSC Clinic Co-director, Sydney Children’s Hospital; Dr David Mowat, Clinical Geneticist and TSC Clinic Co-director, Sydney Children’s Hospital
Family review provided by: Miriam and Curt Chalk, Debbie Crosby, Miia Groenewald, Jeremy and Shell Lumby, Sally Nicholson
Editorial support: Teresa Llewellyn-Evans
Publication was made possible thanks to the financial support of nib foundation.

DISCLAIMER
Please note that the information provided in this publication is not medical advice. You should consult your doctor(s) before taking any action based on any information published by TSA.







